Best Sex Position for Pregnancy: Exploring the Journey to Parenthood
For many couples, achieving pregnancy represents more than just a medical goal—it is a significant, life-altering milestone that brings anticipation and hope for the future. In the midst of this excitement, however, questions often arise about the best ways to optimize the chances of conception. These questions can range from practical concerns about timing intercourse to more intimate matters related to comfort, emotional readiness, and sexual positioning, including the best sex position for pregnancy. Since the human body is influenced by a multitude of factors—hormonal fluctuations, overall health, even stress levels—gaining a fuller understanding of these elements can help alleviate anxieties and foster greater confidence as partners embark on the path toward parenthood.
One area that frequently draws attention is the relationship between physical intimacy and fertility. While reproductive biology has its natural mechanisms, certain practices and considerations—like paying closer attention to ovulation or experimenting with various sexual positions—can potentially provide a small boost to the likelihood of conception. Equally critical, though, is the emotional dimension of trying to conceive. When couples maintain open communication, share their excitement and worries, and support each other through moments of uncertainty, they create an environment where both partners feel valued and understood. This positive emotional space can be especially helpful in navigating any challenges that may arise along the way [1].
Factors That Affect Conception
Individuals often wonder about the best position to get pregnant or whether specific habits can boost fertility. While body alignment can play a minor role, several elements ultimately determine successful fertilization. Key among them is timing intercourse around ovulation, which often occurs mid-cycle. Hormonal imbalances, blocked fallopian tubes, or low sperm count can also impede fertilization. Lifestyle factors—like balanced nutrition, moderate exercise, and stress management—are crucial. Chronic tension disrupts hormones, and age-related shifts in egg and sperm quality should be acknowledged [2].
Physical Alignment Considerations
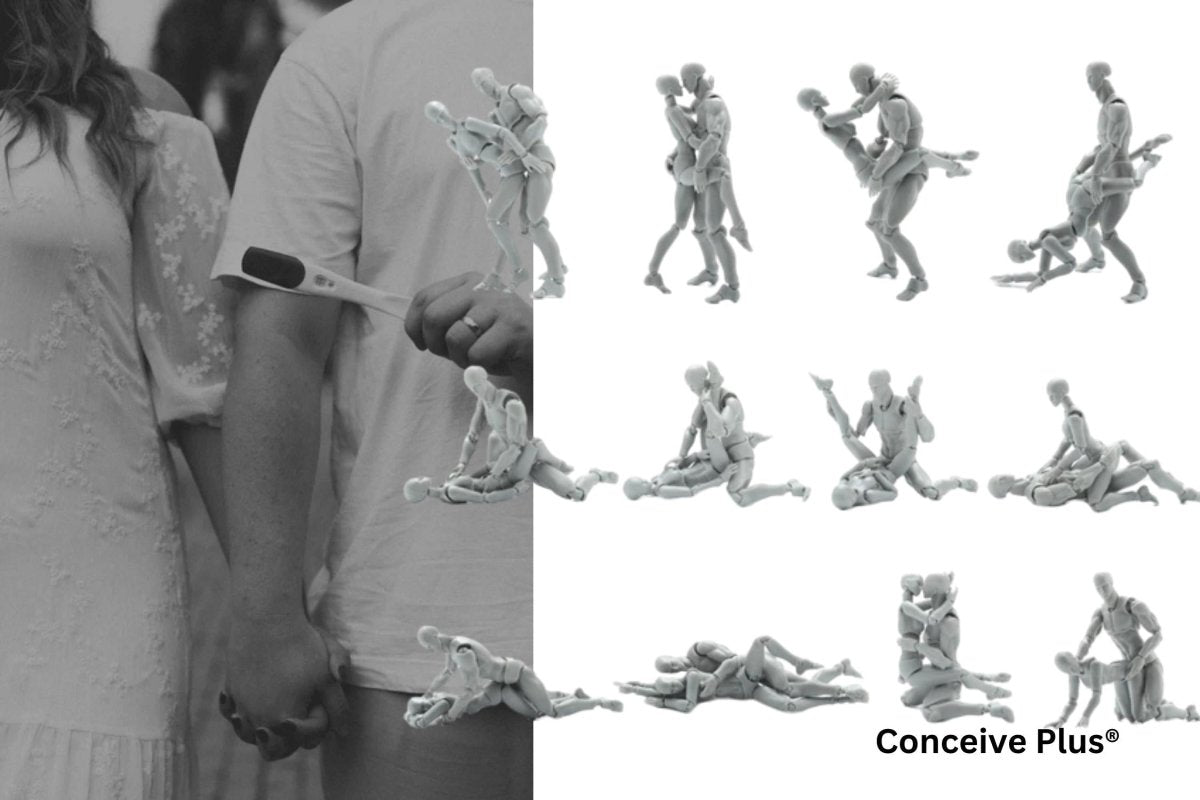
The idea of a pregnant position that ensures rapid conception can be tempting. Experts sometimes suggest that angles allowing deeper penetration may place sperm closer to the cervix. Still, the internal environment of the female reproductive tract is quite dynamic. Sperm can survive multiple days, so exact angles rarely dictate success. Nevertheless, comfort and ease can reduce stress and foster emotional closeness, both beneficial when trying to conceive [3].
Dispelling Common Myths
Frequent discussions about sex positions for pregnancy often give rise to misconceptions. A popular myth is that standing makes conception impossible because gravity hinders sperm movement. In reality, sperm cells are active swimmers that can navigate through the reproductive tract regardless of position. Another myth centers on pillows under the hips significantly boosting the odds. Though mild elevation may momentarily pool fluids near the cervix, it provides only limited benefit. Worrying excessively about technique can transform an intimate experience into a pressured endeavor, undermining enjoyment [4].
Practical Tips for Alignment
Couples exploring positions to get pregnant can focus on maintaining relaxation, emotional harmony, and open dialogue. For some, best positions for conception may involve deeper penetration, but each person’s comfort should guide experimentation. After intercourse, lying still for a few minutes could marginally help sperm remain near the cervix. However, every body shape and preference is unique, so a flexible approach often yields the best results.
For those wondering if specific techniques or positions can influence the gender of your baby, you might be interested in learning more about what sex position helps conceive a girl, which explores how timing and position may play a role in gender conception.
Lifestyle and Health
While alignment can help, broader health factors often play a more significant role. Eating nutrient-rich foods supports egg and sperm quality, while excessive caffeine or alcohol can impede fertility. Moderate exercise aids weight management and circulation. However, overly intense workouts that lead to extreme weight loss or exhaustion may negatively affect reproductive health. Emotional well-being is also vital, as chronic stress can unbalance hormones and disrupt ovulation or sperm production. Identifying stressors and seeking help—whether from a counselor or supportive friends—can be transformative [5].
Emotional Connection
In discussions of positions to conceive, emotional rapport is sometimes overlooked. Feeling safe and valued during intimacy can heighten arousal and encourage a more favorable physiological response. Clear communication about boundaries and preferences helps prevent pain or discomfort, ensuring that intercourse remains pleasurable rather than stressful. Unity during this chapter can bolster confidence and resilience, even if challenges arise.
Refining Techniques
Those curious about the best sexual position for pregnancy might tweak familiar positions instead of adopting unfamiliar methods. Adjust leg placement, use pillows for support, or allow ample time for foreplay to promote natural lubrication and reduce discomfort. Recognizing that the cervix changes position throughout the cycle might guide occasional adjustments. Yet no single action guarantees quick success, and a more holistic view—integrating physical pleasure, emotional harmony, and healthful habits—remains most effective.
For those curious about whether the positioning after intercourse can impact conception, you may want to explore this article on how long to keep legs up to get pregnant, where we examine the potential effects of leg elevation on pregnancy chances.
Medical Insight
In addition to experimenting with a position for pregnancy, couples can support their efforts by considering supplements like folic acid and vitamin D. Adequate sleep also promotes hormonal regulation. If irregular cycles, pelvic pain, or concerning semen analysis results emerge, consulting a doctor is wise. Early intervention can address fertility barriers and prevent prolonged stress [6].
Respecting Partner Needs
Learning how to have pregnant intercourse may bring up differences in comfort or expectations. Respectful communication ensures both partners feel heard and avoids reducing intimacy to a mere task. Scheduling moments of closeness purely for enjoyment can counterbalance the pressure of timing intercourse. Each journey is unique—while some conceive swiftly, others face more extended paths that require patience and support. By voicing concerns and celebrating small successes, couples can maintain unity even amid uncertainty.
Holistic Approaches
Mindfulness can soothe both body and mind, lowering stress and supporting hormonal balance. Light activities like yoga can enhance flexibility and relaxation, while massage may reduce tension and increase bonding. Consistency in intercourse—every two or three days—helps ensure fresh sperm supplies, yet imposing rigid schedules may stifle desire. A balance between frequency and spontaneity fosters optimism and preserves intimacy.
Additional Insights and Guidance
Beyond these core considerations, many couples benefit from exploring complementary strategies that encourage a healthier, more receptive environment for conception. For instance, understanding the nuances of hormonal shifts can offer clarity on why specific days are more fertile. Some individuals choose to track basal body temperature or cervical mucus changes, identifying the window when the egg is most likely to be released. Using ovulation predictor kits can also remove guesswork, helping couples time intercourse more precisely. Nonetheless, focusing too heavily on monitoring can lead to stress, so a balanced approach remains critical.
On the subject of mental well-being, acknowledging that each person’s emotional journey may differ can foster mutual compassion. Some partners might feel eager and optimistic, while others experience anxiety over potential setbacks. Maintaining open dialogue about these feelings can defuse tension and strengthen the bond needed to weather any disappointments. If frustration intensifies, professional counseling can create a safe space to process emotions and reframe the experience in a constructive manner.
In cases where natural methods prove insufficient, medical support may be necessary. Modern advancements include medications to stimulate ovulation, such as clomiphene citrate or letrozole, which can address hormonal imbalances. Intrauterine insemination, where sperm are placed directly into the uterus, may enhance the odds when mild male-factor infertility or cervical issues are present. More complex scenarios might call for in vitro fertilization. This procedure involves retrieving eggs, fertilizing them with sperm in a lab, and transferring resulting embryos to the uterus. Though often seen as a last resort, such options give hope to those facing challenging fertility barriers. Consulting with a reproductive endocrinologist to discuss these possibilities can provide valuable clarity and reassurance.
Meanwhile, alternative therapies may serve as supportive measures alongside conventional approaches. Acupuncture, for example, has garnered attention for potentially improving blood flow to reproductive organs and reducing stress levels. Herbal remedies and dietary supplements, although sometimes lacking extensive scientific validation, may still assist certain individuals by promoting relaxation or improving overall vitality. It remains essential to seek guidance from trained professionals before adopting unproven therapies, as some substances can interfere with prescription medications or complicate underlying conditions.
Another dimension frequently overlooked is the role of social support systems. Friends and family, especially those who have navigated similar challenges, can offer empathy and advice that eases isolation. Online communities and local support groups further expand opportunities for connection, enabling individuals to share stories of triumphs and disappointments without judgment. Learning from others’ perspectives can spark fresh ideas and reinforce the notion that setbacks are often temporary obstacles rather than permanent roadblocks.
Many couples also benefit from a more patient outlook, recognizing that conception may not happen immediately. Statistics indicate that a significant percentage of healthy couples can take up to a year to conceive. This extended timeline can feel discouraging, but understanding it as a normal range can alleviate self-blame. Persisting with balanced lifestyle choices, consistent yet relaxed intimacy, and practical medical supervision sets a reliable foundation for eventual success.
Finally, it is important not to overlook the dimension of self-care. Transitioning from couplehood to parenthood can be an intense process filled with physical and emotional demands. Creating routines that nurture each partner, such as shared walks, mindful breathing exercises, or simple moments of playful connection, can transform potential frustration into productive bonding. Setting realistic expectations—both for fertility goals and relationship dynamics—helps preserve motivation and contentment. In this way, each step of the journey contributes to a strong framework for the new life being welcomed.
The Bottom Line
Discovering the best sex position for pregnancy is a personal choice shaped by comfort, connection, and knowledge. Embarking on the quest to conceive involves hope, curiosity, and sometimes anxiety. While body positioning can offer minor advantages, the broader picture includes emotional fulfillment, communication, and a balanced lifestyle. Fostering trust and well-being can smooth the path, whether or not specific angles prove beneficial. Each couple’s journey unfolds differently, and professional guidance can clarify uncertainties. Above all, maintaining empathy and mutual reassurance can nurture a supportive environment for conception.
References
- Lawrenz B, Ata B, Kalafat E, Del Gallego R, Selim S, Edades J, Fatemi H. Undetected, natural conception pregnancies in luteal phase stimulations-case series and review of literature. Hum Reprod. 2024 Oct 1;39(10):2268-2273. doi: 10.1093/humrep/deae165. PMID: 39018559.
- Wilcox AJ, Baird DD, Weinberg CR. Time of implantation of the conceptus and loss of pregnancy. N Engl J Med. 1999 Jun 10;340(23):1796-9. doi: 10.1056/NEJM199906103402304. PMID: 10362823.
- Lee JT, Lin CL, Wan GH, Liang CC. Sexual positions and sexual satisfaction of pregnant women. J Sex Marital Ther. 2010;36(5):408-20. doi: 10.1080/0092623X.2010.510776. PMID: 20924936.
- Sacomori C, Cardoso FL. Sexual initiative and intercourse behavior during pregnancy among brazilian women: a retrospective study. J Sex Marital Ther. 2010;36(2):124-36. doi: 10.1080/00926230903554503. PMID: 20169493.
- Wesołowska E, Jankowska A, Trafalska E, Kałużny P, Grzesiak M, Dominowska J, Hanke W, Calamandrei G, Polańska K. Sociodemographic, Lifestyle, Environmental and Pregnancy-Related Determinants of Dietary Patterns during Pregnancy. Int J Environ Res Public Health. 2019 Mar 2;16(5):754. doi: 10.3390/ijerph16050754. PMID: 30832307; PMCID: PMC6427254.
- Pérez-López FR, Pilz S, Chedraui P. Vitamin D supplementation during pregnancy: an overview. Curr Opin Obstet Gynecol. 2020 Oct;32(5):316-321. doi: 10.1097/GCO.0000000000000641. PMID: 32487800.



















