Why Am I Ovulating So Much: Understanding Perceived Frequent Ovulation

The female reproductive cycle is a finely tuned process that revolves around ovulation—the release of a mature egg from one of the ovaries. Typically, this event happens once per menstrual cycle, roughly in the middle of that cycle. However, some individuals find themselves wondering, why am I ovulating so much, or if they are ovulating more often than usual. This perception can stem from a variety of factors, including heightened awareness of bodily signs, changing hormonal balances, or physical symptoms that can be easily confused with the real ovulatory window. It is often a source of both curiosity and concern, as one might associate multiple ovulations with issues of fertility, irregular cycles, or other health conditions. Yet to truly assess whether you’re experiencing actual multiple ovulatory events or just perceiving them more intensely, it’s necessary to explore the underlying biological processes, potential causes, and ways to interpret common signals, such as a noticeable increased cervical discharge.
The Body’s Ovulatory Process and Standard Rhythms
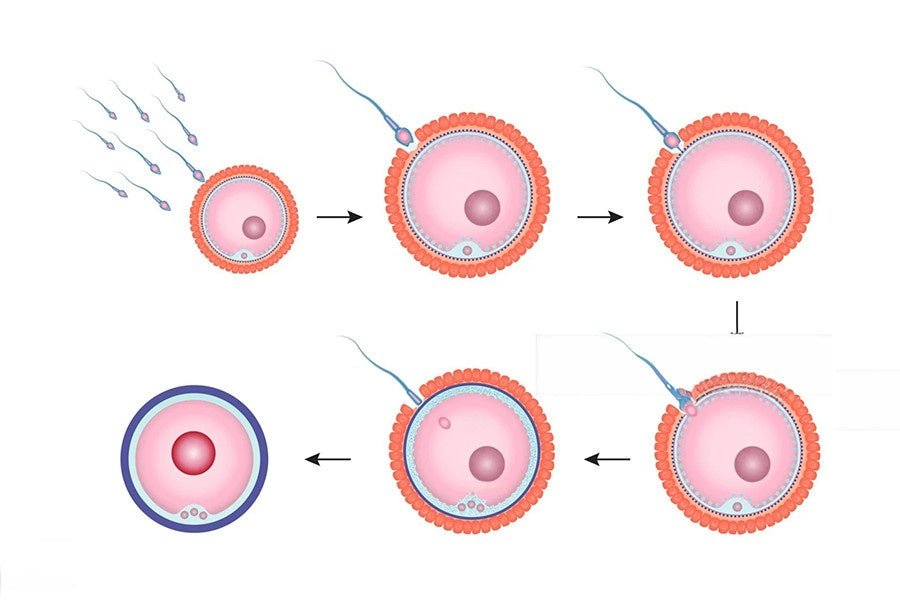
Ovulation is governed by a cyclical interplay of hormones. Early in the menstrual cycle, the pituitary gland secretes follicle-stimulating hormone (FSH), encouraging follicles on the ovaries to develop. One follicle typically becomes dominant, nurturing a mature egg. Around the midpoint of the cycle—often day 14 in a textbook 28-day cycle but highly variable among individuals—a surge in luteinizing hormone (LH) triggers ovulation. After the egg is released, the remnant follicle transforms into the corpus luteum, producing progesterone to prepare the uterine lining for potential implantation. If no fertilization occurs, hormone levels drop, leading to menstruation and the start of a new cycle [1].
In reality, true multiple ovulations in a single cycle, known as hyperovulation, are relatively rare. Some research suggests it can happen in certain cases, potentially leading to fraternal twins if both released eggs are fertilized. However, many who believe they are ovulating more often than average may actually be experiencing normal fluctuations in the signs their body produces. For example, sensations like lower abdominal cramping or changes in discharge might appear at different times for each cycle or intensify under certain conditions [2]. Some individuals may also experience ovulation cramps on both sides during their cycle, which can sometimes create the impression of multiple ovulations when, in reality, it’s often a normal response to ovarian activity rather than separate egg releases.
Possible Reasons for Feeling Like You’re Ovulating Frequently
A common explanation for why someone might sense that they are ovulating repeatedly is simply improved self-awareness. Individuals trying to conceive or prevent pregnancy often track basal body temperature, cervical mucus changes, and use ovulation predictor kits. Enhanced focus on these observations can give the impression of repeated fertility windows. Additionally, stress or lifestyle shifts can make bodily cues more pronounced. A new exercise regime might introduce twinges in the pelvic region, potentially mistaken for additional ovulatory pains [3].
Fluctuating hormone levels also contribute. If estrogen peaks more significantly, there may be a marked increase in the physical signs associated with ovulation. This may prompt someone to think, “Am I ovulating again?” even when it’s just one event with a pronounced hormonal signature. Similarly, some people have longer cycles that create more days of fertile cervical mucus, intensifying the sense that ovulation keeps lingering. Ultimately, while the body typically adheres to a single major LH surge per cycle, various bodily indicators can blur the lines between the pre-ovulatory and post-ovulatory phases, leading to confusion.
The Role of Hormonal Variability and Health Conditions
Certain medical conditions can affect how often someone appears to ovulate or at least how their body displays ovulatory symptoms. Polycystic ovary syndrome (PCOS) is one example. Characterized by hormone imbalances and irregular cycles, PCOS can alter the pattern of follicle development. Some with PCOS have persistent or fluctuating estrogen levels, leading to repeated attempts at follicular growth and ovulation without a definitive egg release. This might manifest as multiple episodes of fertile-like cervical mucus throughout a single cycle. For those looking to promote regular ovulation and support hormonal balance, supplements like Conceive Plus Ovulation Support, which contains Myo-Inositol, D-chiro Inositol, and essential nutrients, can be a beneficial addition to reproductive health routines.
Other hormonal disruptions, such as thyroid disorders or hyperprolactinemia, can also cause irregularities that might be misread as frequent ovulation. If the thyroid is underactive or overactive, it can influence the delicate dance of reproductive hormones. As a result, signs like cramping, or changes in cervical fluid, may occur sporadically rather than in one consistent window. For individuals with elevated prolactin levels, ovulation can become sporadic or even absent, leading them to interpret any cyclical symptom as another ovulation attempt. These scenarios highlight how underlying medical complexities might explain confusing patterns rather than true multiple egg releases each cycle.
Lifestyle Influences: Stress, Exercise, and Nutrition
Physical and emotional well-being also shape the ovulatory process. Heightened anxiety or prolonged stress elevates cortisol, which can disturb the hormones that regulate the menstrual cycle. In certain instances, this might delay or shorten phases of the cycle, increasing the difficulty of pinpointing where ovulation precisely happened. If the cycle’s length changes unpredictably, a person may track bodily cues incorrectly, concluding that multiple ovulations are occurring in the same month.
Strenuous or newly adopted workouts also play a part. Intense exercise routines, particularly those that significantly reduce body fat, can disrupt regular ovulatory function. Conversely, adopting moderate, balanced exercise might help regulate cycles by stabilizing hormone levels. Diet and nutrition are equally vital—insufficient caloric intake or a lack of key nutrients can compromise overall endocrine balance. Thus, if someone’s workout regimen or dietary habits shift and they notice new or stronger pelvic sensations, it may be more a sign of stress on the body than a genuine spike in egg release frequency.
Interpreting Changes in Cervical Discharge
One of the most obvious fertility signals is cervical mucus. Before ovulation, rising estrogen triggers a transformation in mucus consistency from thick and sticky to watery and stretchy, resembling raw egg whites. This fluid fosters sperm motility, aiding their journey through the cervix. After ovulation, progesterone thickens the mucus again, forming a barrier that helps prevent additional sperm from entering. However, the phrase increased cervical discharge can mean different things in various contexts. If an individual notices more fluid during multiple parts of their cycle, they might worry they are repeatedly ovulating.
In reality, frequent fluctuations in cervical discharge don’t always signify new egg releases. Occasionally, random hormonal shifts or mild infections can alter the fluid’s texture and volume. Moreover, some individuals simply produce more fluid overall, which might remain watery for longer. Paying attention to the color, odor, and associated sensations can help differentiate normal cervical mucus changes from potential issues like bacterial vaginosis or yeast overgrowth. Should any symptoms like itching or irritation accompany the fluid changes, it’s advisable to seek medical advice.
Monitoring for Ovulatory Disorders
Although multiple ovulations in one cycle are uncommon, it’s never a bad idea to track patterns for clarity, especially if a person suspects irregularities. Tools like daily basal body temperature recordings offer a precise look at luteal phase changes. A noticeable temperature shift upward often indicates ovulation has occurred. Meanwhile, ovulation predictor kits measure LH surges in urine. If these kits continuously show positives for a prolonged span, it may point to an underlying hormonal imbalance.
Medical consultations become especially important if one experiences severe pain or other disruptive symptoms. Recurring bouts of intense pelvic cramping at various times in the cycle might hint at conditions like endometriosis or ovarian cysts. If found early, these conditions can be managed or treated effectively. Conversely, ignoring perplexing signs for too long might result in prolonged discomfort or missed opportunities for early intervention. Ultimately, open communication with a gynecologist can demystify confusion about ovulation frequency and illuminate potential next steps [4].
The Bottom Line
Ultimately, it’s common to ask why am I ovulating so much when noticing extra or unfamiliar bodily cues, but understanding the intricacies of the menstrual cycle often reveals that the system is following its usual rhythmic dance. All in all, while it’s unusual for people to ovulate multiple times in a single menstrual cycle, various factors can lead to the impression of frequent egg release. Shifting hormone levels, heightened body awareness, and fluctuating physical symptoms like increased cervical discharge can blur the lines between a single ovulatory event and what might appear as two or more. In many cases, the body is simply showcasing normal cyclical changes in a pronounced way. With thorough tracking and, if necessary, professional evaluations, individuals can demystify these signals and address any underlying concerns.
References:
- Su HW, Yi YC, Wei TY, Chang TC, Cheng CM. Detection of ovulation, a review of currently available methods. Bioeng Transl Med. 2017 May 16;2(3):238-246. doi: 10.1002/btm2.10058. PMID: 29313033; PMCID: PMC5689497.
- Dyer O. Women may ovulate two or three times a month. BMJ. 2003 Jul 19;327(7407):124. PMCID: PMC1126506.
- Cohen J, Iffy L, Keyser HH. Basal body temperature recordings in spontaneous abortion. Int J Gynaecol Obstet. 1976;14(2):117-22. doi: 10.1002/j.1879-3479.1976.tb00579.x. PMID: 10200.
- Dyer O. Women may ovulate two or three times a month. BMJ. 2003 Jul 19;327(7407):124. PMCID: PMC1126506.